Important takeaways on vasculitis and COVID-19 vaccines from Dr. Joanne Jiang’s presentation at the 2021 VFC AGM on April 17, 2021
In case you missed Dr. Jiang’s presentation during the 2021 VFC AGM, or you need a refresher, here are some of the key takeaways that vasculitis patients need to keep in mind with regards to the COVID-19 vaccinations. Please note: This information is based on the best available information as of April 17, 2021.
-
Individuals with autoimmune disease (including vasculitis) are more likely to have a more severe form of COVID-19 infection.
-
Vaccine efficacy and its ability to provoke an immune response (immunogenicity) in immunosuppressed individuals is uncertain, but is expected to be lower than what is observed in the general population.
-
Factors associated with increased severity of COVID-19 infection in vasculitis patients:
from a small study of 65 patients (UK/Ireland study):
-
Prednisone use (any dose)
-
Lung disease
-
Disease activity and other immunosuppressives were not associated with severe COVID-19 outcomes in this particular study, however another study done on 3729 patients (with variable rheumatic conditions) found that these factors were associated with increased odds of death related to COVID-19 infection.
-
A recently published study in Lancet Rheumatology found you’re more likely to have severe COVID symptoms if you received rituximab last in the last 50 days or so (with some up to 100 days), and you also have a higher risk of dying from COVID within that same timeframe.
-
Do I need to bring a formal doctor signed letter to get the vaccine? No. Some places may ask you to fill out an attestation form with your physician’s information, but it DOES NOT need to be filled out by your physician UNLESS a signature is needed, and this appears NOT to be required so far. In Ontario, the ORA (Ontario rheumatology association) has officially confirmed that attestation letters from physicians are NOT needed and is actually acting as a barrier to vaccination.
-
Can I request a shorter interval for the 2nd dose? No, not yet for vasculitis patients! This is determined by Ministry of Health, in Ontario visit: https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/vaccine/COVID_19_medical_exceptions_vaccine_dose_intervals.pdf
Current exempted special populations only include: transplant (solid organ, or stem cell), and those receiving chemotherapy or immunotherapy for cancer, NOT vasculitis!
-
Which Vaccine should I get? The first vaccine, approved for you, that you can get, is the best vaccine to get! The most important thing is that they all prevent hospitalization and death. All approved vaccines in Canada reduce the severity and hospitalizations due to COVID-19 infection, and virtually eliminate the risk of death for those in the general population.
-
Most clinical trials often exclude people with autoimmune diseases and those on immunosuppressive treatment including those with cancer, transplants, chronic infections, pregnancy and children are usually excluded in early studies.
-
Early data from a John Hopkins study shows that individuals with autoimmune disease can produce antibody response even after 1 dose of the vaccine. However, only 2 had vasculitis (out of 123), Methotrexate did not negatively impact antibody development.
Rituximab and MMF (mycophenolate/cellcept), did affect antibody development!
-
There remain many unanswered questions! For example, what is the minimum (threshold) COVID-19 antibody titre that is sufficient to prevent active infection, what is the vaccine response in those who have TOO FEW immunoglobulins (hypogammaglobulinemia), what is the vaccine response in those who produce TOO MANY immunoglobulins (hypergammaglobulinemia), is there a role for a 3rd shot (aka 2nd booster) in immunocompromised populations?
-
Timing of vaccination, and timing of immunosuppressive treatment may vary, see chart below as a reference, and consult with your rheumatologist for your individual recommendation.
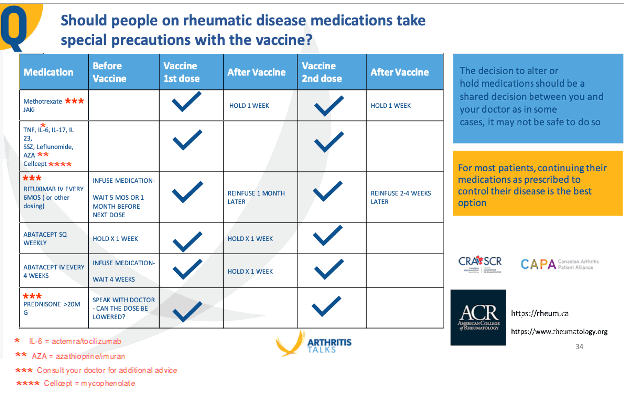
Note: Patients on some immunosuppressive therapies may have reduced protection from the COVID-19 vaccines. However, given the overall benefit of the COVID-19 vaccines the benefits of vaccination will still be large for most vasculitis patients. Furthermore, even a little bit of protection is better than no protection at all! Continuing medications will often be the safest option to prevent disease flares until more evidence is available. There is no scientific agreement on when the best time is to get the COVID-19 vaccines when you are on Rituximab.
-
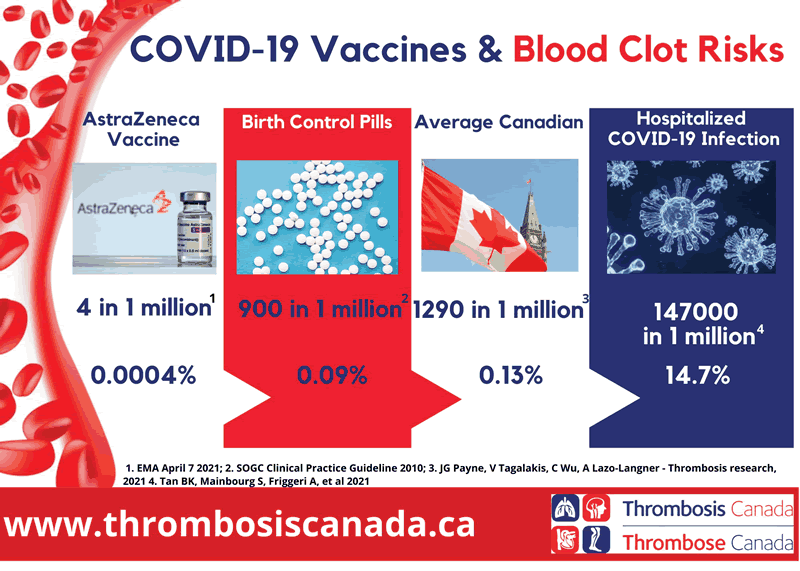
See the chart below to compare the lower risk of blood clots compared to the higher risk of COVID-19 disease! Thrombosis Canada concludes: “The benefits of preventing blood clots and other disease caused by COVID-19 far outweigh any possible risks [of vaccination], which we consider very low.”
-
Things to do:
– Sign up for the first COVID-19 vaccine available to you.
– Discuss holding or delaying of medications with your specialists.
– Remember that the guidelines & recommendations exist in an IDEAL situation, but the real world is full of surprises!
– Continue to take personal health measures to protect yourself from COVID-19 exposure, even after receiving the vaccine.
-
Don’t do the following:
-
Delay or hold treatment if your vasculitis is active
-
Stop prednisone abruptly without discussing with your specialists, especially if your dose of prednisone is 5mg or greater.
If you are interested in the journal references used in this website post please reach out [email protected] for additional information.
The vasculitis community is at increased risk to COVID-19, keep safe and take extra precautions in these challenging times.
Jon Stewart
President
Vasculitis Foundation Canada
